All published articles of this journal are available on ScienceDirect.
Concerns Related to Neuraxial Anesthesia and the Impact of Patient Education among Women Undergoing Cesarean Section in Saudi Arabia
Abstract
Background
Neuraxial anesthesia is widely recognized as the most effective technique for cesarean pain management. However, some concerns persist, particularly regarding post-spinal backache, pain at the needle insertion site, or headache post-operatively. While numerous studies have explored clinical concerns related to obstetric anesthesia, there remains a notable gap in research specifically addressing the psychological effects associated with these concerns.
Methods
The study employed a cross-sectional analytical design among obstetric patients undergoing elective cesarean section with neuraxial anesthesia. Participants aged between 18 and 45 years were targeted. The data collection tool was a questionnaire (closed-ended questions) using a non-probability convenience sampling technique.
Results
Concerns were reported by 94% of women, with the most common being post-spinal backache. These concerns were not significantly associated with either intraoperative incidences or preoperative anxiety. However, previous exposure to neuraxial anesthesia was significantly associated with a lower rate of refusal. Additionally, the education provided immediately before the procedure was not sufficient.
Discussion
The findings highlight the importance of proactive patient education and public awareness campaigns to address misconceptions about neuraxial anesthesia, enhance understanding, and support informed decision-making among obstetric patients.
Conclusion
Neuraxial anesthesia raises several concerns among obstetric patients, affecting 94% of them. These concerns were not significantly associated with specific intraoperative events such as bradycardia, nausea, and vasovagal syncope, either with preoperative anxiety or the education provided. However, previous exposure to neuraxial anesthesia was associated with a lower rate of refusal among pregnant women.
1. INTRODUCTION
The most prevalent surgical birth method worldwide is the Caesarean Section (CS). Following fetal viability, a CS involves cutting the abdomen and uterus to deliver the fetus, membrane, and placenta [1].
Few decades, the prevalence of cesarean deliveries has sharply increased globally. In fact, while the frequency of vaginal deliveries is declining, it is clear that cesarean deliveries have become an epidemic phenomenon in various regions of the world [2].
The best technique for reducing labor pain is neuraxial analgesia during cesarean section [3]. It almost completely relieves labor pain from (90–95%) [4]. Spinal, epidural, and combined spinal and epidural anesthesia are the three types of neuraxial analgesia that can be used in cesarean section surgeries [5-7].
Even though neuraxial analgesia for childbirth has improved dramatically, there are still many fears and misunderstandings about this topic [8, 9]. Previous studies have shown that many pregnant women refuse or hesitate to do neuraxial analgesia because of falsely believing that this procedure will lead to many postoperative problems, such as post-spinal backache, intraoperative pain, and residual paralysis [10, 11]. Although neuraxial analgesia is efficient and frequently used during cesarean section, little is known about how well it is accepted by pregnant women [12-16].
Around the world, many studies have addressed the concerns associated with obstetrics; nevertheless, there is a lack of research describing their psychological impacts. In this study, we aimed to investigate the effects of concerns associated with neuraxial anesthesia and their relationship with preoperative anxiety and intra-operative incidences. Furthermore, we aimed to analyze the value of educating pregnant women about neuraxial blockade in improving postoperative patient satisfaction.
2. METHODS
The study was conducted using a cross-sectional analytical design. The study took place in the Department of Obstetrics and Gynecology and the operating rooms in King Abdulaziz Medical City. The participants included 135 individuals, and the sample size was determined using Raosoft, an online sample calculator. Approximately 1 to 3 cases were collected daily over a period of 7 months. Hence, our estimated sample size was 132, given a confidence interval of 95%, a margin of error of 5%, a population size of 200, and a response distribution of 50%. In this study, a non-probability convenience sampling technique was utilized. Physical questionnaires were distributed to obstetric patients undergoing cesarean sections with neuraxial blockade (spinal or epidural) based on their availability.
The questionnaire was adapted from the studies of Al Mousa et al. [17] and Taman and Hegazy [11] with some modifications. It was validated and reassessed. The questionnaire comprised two sections. The first section was intended for the patient and contained two parts: preoperative and postoperative. The preoperative part included questions about the patient's demographic data, such as age, education level, and employment, while the postoperative part assessed patient satisfaction after the surgery. The second section, which focused on anesthesia-related data, included documentation of intraoperative events such as bradycardia, nausea, and vasovagal syncope, as well as the methods used for anxiety management. Non-pharmacological techniques, such as music therapy, guided breathing, and verbal reassurance, were employed when appropriate. This section was completed by the anesthesia staff involved in the case.
The questionnaire was filled out by staff members. For the first section, which focused on preoperative information, the staff asked the obstetric patients questions before surgery and recorded their responses. After the surgery was completed, the same staff members returned to the patients in the recovery area to collect responses to the postoperative questions. The second section of the questionnaire contained intraoperative data, which was filled out entirely by the staff based on observations and clinical records during the procedure.
After receiving approval from the institutional review board of King Abdullah International Medical Research Center (KAIMRC), a pilot test was employed to assess the validity and reliability of the questions. We included all obstetric patients between 18 and 45 years old undergoing elective cesarean sections with neuraxial anesthesia. Data were collected in Excel and analyzed using IBM SPSS Statistics software. Categorical variables were presented as frequency and percentage, while continuous variables were presented as mean and standard deviation. Chi-square tests were used to compare categorical variables. p-values < 0.05 were considered significant. Cases converted to general anesthesia were excluded from the study, and any missing data were categorized as “Not answered.
3. RESULTS
The study included 135 patients undergoing elective cesarean section with neuraxial anesthesia. Two cases were excluded due to conversion to general anesthesia (Fig. 1).
The most common age group was 31–35 years, representing 34% of the total sample. Of the participants, 51% had a previous cesarean section, while 47% were undergoing their first. Additionally, 47% had previously received neuraxial anesthesia, 47% were experiencing it for the first time, and 5% were not sure.
A total of 94% of women reported concerns regarding neuraxial anesthesia, with the most common concern being post-spinal backache (Table 1). In contrast, just 5% did not have any concerns regarding neuraxial anesthesia. The education process was perceived from two sources: information was obtained either directly from the doctor or anesthesia team, or through self-learning via social interactions or internet searches. The percentage of women educated by the anesthesia team was 85%, while self-learning accounted for 58% (Table 2).
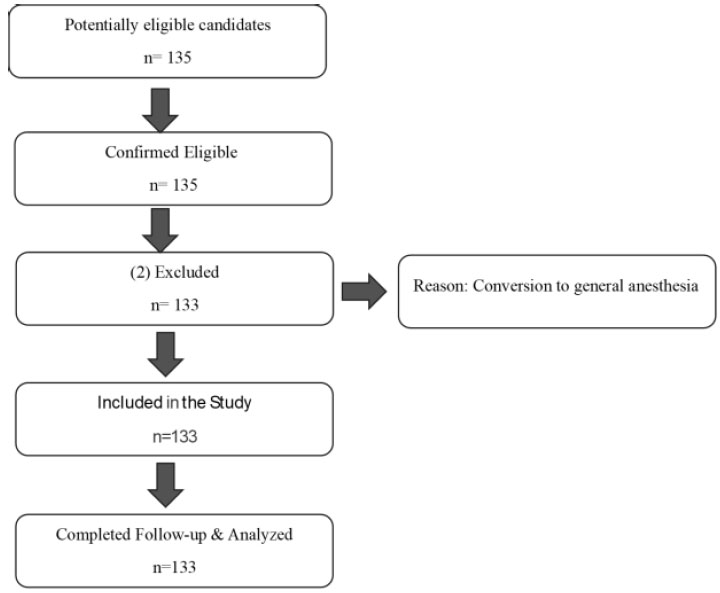
This flow diagram illustrates the selection process of participants in the study.
| Concern | Frequency | Percentage % |
|---|---|---|
| Post-spinal backache | 84 | 62.2% |
| Needle prick pain | 57 | 42.2% |
| Residual paralysis | 46 | 34.1% |
| Nausea and vomiting | 44 | 32.6% |
| Headache | 42 | 31.1% |
| Fetal distress | 26 | 19.3% |
| Advice from relatives | 17 | 12.6% |
| Hair loss | 10 | 7.4% |
| Not sure | 8 | 5.9% |
| Slows labor | 4 | 3.0% |
| Breastfeeding difficulty | 1 | 0.7% |
| Pregnant characteristic | Number | Percentage |
|---|---|---|
| Age | ||
| 18-25 | 19 | 14.1% |
| 25-30 | 1 | 0.7% |
| 26-30 | 32 | 24.1% |
| 31-35 | 47 | 34.8% |
| 36-40 | 22 | 16.3% |
| 41-45 | 12 | 8.9% |
| BMI_category | ||
| Normal | 60 | 45.1% |
| Overweight | 39 | 29.3% |
| Obese | 32 | 24.1% |
| Not answered | 2 | 1.5% |
| Residency | ||
| Not answered | 1 | 0.7% |
| Rural | 22 | 16.3% |
| Urban | 110 | 82.7% |
| Employment | ||
| Empolyed | 56 | 42.1% |
| Unemployed | 77 | 57.9% |
| Education level | ||
| High school | 45 | 33.3% |
| Less than high school | 8 | 5.9% |
| Postgraduate | 11 | 8.2% |
| Undergraduate | 69 | 51.9% |
| First Child? | ||
| Yes | 41 | 30.8% |
| No | 92 | 69.2% |
| History of cesarean section | ||
| Yes | 68 | 51.1% |
| No | 64 | 47.4% |
| Not answered | 1 | 0.7% |
| How many children do you have? | ||
| 0 | 39 | 29.3% |
| 1 | 15 | 11.1% |
| 2 to 3 | 48 | 36.1% |
| 4=< | 31 | 23.0% |
| First neuraxial anesthesia? | ||
| Yes | 63 | 47.4% |
| No | 63 | 47.4% |
| Not sure | 7 | 5.2% |
| Any concerns from relatives or friends regarding neuraxial anesthesia? | ||
| yes | 125 | 94.0% |
| No | 8 | 5.9% |
| Did you receive any education from a medical professional? | ||
| Yes | 114 | 85.7% |
| No | 19 | 14.1% |
| Did you search or read about the neuraxial blockade? | ||
| Yes | 79 | 58.5% |
| No | 54 | 40.6% |
| Any chronic disease? | ||
| Yes | 31 | 23.0% |
| No | 102 | 76.7% |
| Compared Variables | Pearson Chi-square | p-value |
|---|---|---|
| Having concerns With Intraoperative Incidence |
2.101 | 0.147 |
| Having concerns With Experiencing preoperative anxiety |
3.140 | 0.076 |
| Had received previous education With Satisfaction level |
5.804 | 0.122 |
| First exposure to a neuraxial block With Having concerns |
5.724 | 0.057 |
| First exposure to a neuraxial block With Refusal of neuraxial blockade |
30.097 | 0.0001* |
* Association is significant.
Ninety-one percent of patients experienced preoperative anxiety, and 45% of these were managed using non-pharmacological methods such as music therapy, breathing techniques, and reassurance. Fifty-seven percent of women required convincing by the anesthesia team to undergo neuraxial anesthesia. The most reported pain score was between 4 and 6, representing 37% of respondents. For future deliveries, 78% of women stated they would request neuraxial anesthesia again, and only 18% would not. Following delivery, 71% of patients were satisfied with the services provided at King Abdulaziz Medical City in Jeddah, Saudi Arabia, while only 6% were dissatisfied, and 21.8% were neutral.
After using the chi-square test to assess the association between concerns and intraoperative incidence and preoperative anxiety, the results showed that the concerns were not significantly associated with either intraoperative incidence or preoperative anxiety. Additionally, receiving education was not significantly associated with satisfaction level (Table 3). However, previous exposure to neuraxial anesthesia was significantly associated with refusal of neuraxial blockade (Pearson chi-square = 7.206, p-value = 0.003).
4. DISCUSSION
Our most important finding was that there was no significant relationship between concerns and either intraoperative incidents such as bradycardia, nausea, and vasovagal syncope, or preoperative anxiety. However, women who had received neuraxial anesthesia before showed a lower refusal rate, suggesting that prior experience may help reduce fear and improve acceptance.
In our group of pregnant Arabian women, 94% had at least one concern about neuraxial anesthesia, with the most common concern being back pain after the procedure. Obstetric anesthesia has long been plagued by myths and false information [18]. According to our findings, there have been five studies on awareness of epidural anesthesia in Saudi Arabia. Most of these studies showed low levels of awareness regarding epidural anesthesia, similar to our study, except for the last study conducted in Al Khobar in 2021 at King Fahad University Hospital, which found that most women were aware of using epidural for labor pain reduction [17].
Although 85% of women reported receiving education about neuraxial anesthesia from anesthesia staff and 58% engaged in self-learning, our study found that education immediately before delivery was not significantly associated with reduced concerns or increased satisfaction. Previous studies indicated that fears based on inaccurate information may be alleviated through patient-provided communication and education [10]. In general, obstetric patient satisfaction is high regardless of the patient education method [13]. A study by Hanaa Baagil, Hamzah Baagil, and Mark Ulrich Gerbershagen emphasized that addressing these concerns preoperatively, such as through counseling or anxiety management, has been shown to improve patient satisfaction and reduce the overall demand for anesthetics [19]. We believe the education process immediately before the procedure is not enough to correct misconceptions about neuraxial anesthesia. For example, the study by Brandon M showed that using regular care alone or routine care with a further educational program consisting of three components, a video, a brochure, and in-person counseling, increased epidural use among Hispanic women. The educational program reduced misconceptions regarding epidural analgesia in both Hispanic and non-Hispanic populations [3].
Based on our findings, we did not find studies on the effect of concerns on intraoperative incidences or preoperative anxiety. In our study, there was no significant relationship between them. However, a study by Ariel J. Lang examined the effect of anxiety on pain and showed that anxiety sensitivity (AS), measured by the Anxiety Sensitivity Index, was significantly associated with maximal pain during labor, as well as sensory and affective pain components assessed by the McGill Pain Questionnaire. AS was found to predict both maximal pain and sensory features of pain, surpassing demographic, social, and psychological characteristics such as depression and anxiety [20].
Also, a study by Yun-Yun K. Chen and colleagues found that preoperative anxiety can result in worsened intraoperative outcomes, such as hemodynamic instability and elevated stress levels, which may increase the need for sedation or analgesics during surgery [21]. We found that a high percentage of patients had preoperative anxiety (91%), which is why it is important to identify the causes that could raise anxiety levels, and 45% of cases were managed using non-pharmacological methods.
Therefore, it is essential for the anesthesia team to take proactive steps in educating obstetric patients well in advance of their scheduled cesarean section. This education can include sharing relevant studies and clinical experiences that demonstrate the positive outcomes of neuraxial anesthesia. Furthermore, increasing public awareness through targeted campaigns and distributing concise, informative brochures about the benefits and safety of neuraxial anesthesia can significantly enhance patient understanding and support informed, confident decision-making. This is particularly important due to the current lack of widespread anesthesia awareness campaigns in our country.
Many studies have focused on understanding problems that patients experience from neuraxial anesthesia, such as low back pain, needle prick pain, and residual paralysis. In this study, we assessed the quality of neuraxial anesthesia by describing the relationship between prior exposure to neuraxial anesthesia and its rejection. Our study revealed that women who had tried neuraxial anesthesia before had a lower refusal rate, which reflects improvements in healthcare and anesthesia.
The strengths of this study include that data were extracted directly from pregnant women just before cesarean section in the holding bay. Second, this is one of the first studies to assess the psychological effects of concerns on pregnant women. One of the limitations of the study is that it included patients whose preoperative anxiety was managed using interventions, which may have influenced the results. This could partly explain why previous concerns did not have a significant effect on preoperative anxiety, as some anxiety may already have been reduced prior to the cesarean section. Additionally, the study was conducted only in the western region and did not take variations in other areas into consideration.
CONCLUSION
In summary, while neuraxial analgesia is effective for cesarean pain relief, concerns, especially about post-spinal backache, remain high despite prior education. Our study found no significant link between psychological concerns and intraoperative events or preoperative anxiety. However, prior experience reduced refusal rates. Structured education and improved communication by anesthesia teams are essential to enhance understanding and acceptance.
AUTHORS' CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: A.A.O., M.A.: Study conception and design; M.K., M.A., S.A., W.A.: Data collection; A.Y., A.A., A.H.: Analysis and interpretation of results; E.K., A.I.: Writing the Paper; M.S.B.: Writing - Original Draft Preparation; G.G.M.: Writing - Reviewing and Editing. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| AS | = Anxiety Sensitivity (measured by the Anxiety Sensitivity Index) |
| CS | = Caesarean section |
| IRB | = Institutional Review Board |
| KAIMRC | = King Abdullah International Medical Research Center |
| p-value | = Probability value |
| SPSS | = Statistical Package for the Social Sciences |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
On November 10, 2023, the King Abdullah International Medical Research Center (KAIMRC) authorized this clinical investigation, which was carried out in King Abdulaziz Medical City under Protocol No.SP23J/092/05.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this study are available from the corresponding author upon request.
ACKNOWLEDGEMENTS
The authors would like to extend their sincere gratitude to the Obstetrics Department for their invaluable technical and material support in facilitating student entry into the department and for assisting with the printing of the questionnaire.